Stage 1 SIRS
Welcome back to my series addressing sepsis and why it is important to your cases. Feel free to email me with any questions regarding the information I have provided so far or if you would like some help with your one of your cases.
Today we are talking about SIRS:
- what is systemic inflammatory response syndrome (SIRS), and
- how is SIRS related to sepsis?
In prior posts, we’ve mentioned SIRS and Sepsis. We know that if Sepsis is overlooked or mistreated, sepsis can lead to septic shock, organ failure, and potentially death.
Key facts:
- Because there are no specific tests to diagnose sepsis, it is imperative that nurses do the daily assessments for SIRS and infection
What is systemic inflammatory response syndrome (SIRS)?
Systemic inflammatory response syndrome (SIRS) is a serious condition in which there is inflammation throughout the whole body – an exaggerated defense response of the body to a noxious stressor, including infection, to localize and then eliminate the source of the insult.
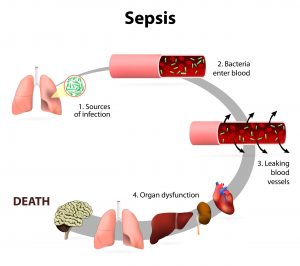
Paige Legal Nurse Consulting knows that the Cardiovascular assessment of a resident/patient is a nurse’s most objective tool to determine the presence of these symptoms and Nursing standard requires it to be done on a daily basis. The first symptoms of SIRS is an elevated heart rate (tachycardia), low blood pressure (hypotension), a low (hypothermia) or elevated temperature, and a low or high white blood cell count. This is because SIRS causes systemic vasodilation, (causing tachycardia (a heart rate above 100) and below baseline blood pressure (hypotension). These are cardinal signs of decompensation requiring immediate attention and interventions because the body can maintain and tolerate a fast heart rate and low blood pressure for only so long before finally giving out.
In a hospital, vital signs are taken every shift (or more often if indicated/ordered). In a nursing home, vital signs are typically done weekly or as ordered. However, if an infection is suspected, nursing should be notifying the medical team and as an assessment be doing more frequent monitoring of a resident’s vital signs.
When monitoring the blood pressure, mean arterial pressure (MAP) is another crucial indicator of perfusion status. Electronic blood pressure machines monitor map readings. The surviving sepsis campaign created a treatment guideline for patients with sepsis and identified a map of less than or equal to 65 mmHg as adequate for supporting organ perfusion. Indicating a MAP of less than 65 mmHg can be a sign that vital internal organs such as brain, heart, kidneys are not being oxygenated and perfused adequately and may suffer permanent damage consequently.
- In any facility type, Nursing does not need a doctor’s order to do vital signs. These can be done at any time at nursing’s discretion as an assessment tool. Standard of care for nursing includes knowing when vital signs should be monitored and reporting results to the medical team.
Now you can better understand why the identification of SIRS symptoms as a basic nursing assessment tool is important in daily nursing care and can be used to avert a medical emergency.
Keep a lookout in your inbox over the next couple of weeks for my emails which will talk about The signs of sepsis in more detail as well as the different areas most noted for sepsis development. I think you’ll find them educational and informative, and ultimately helpful in your cases involving sepsis and death.
Paige Legal Nurse Consulting is a certified Legal Nurse Consulting firm with experienced acute care and nursing home nurses that are qualified to review cases involving infection and sepsis. Call 508-292-2372 or schedule your case development review online with us today!

Christie Paige MSN RN-BC LNC
Christie Paige is a Registered Nurse with over thirty years of experience. She brings her vast and extensive knowledge of clinical practice into the medical-legal arena as a Certified Legal Nurse Consultant. Mrs. Paige is the owner and senior nurse consultant of Paige Legal Nurse Consultants which specializes in Nursing Home cases focused on Sepsis, falls, pressure sore injuries and elder care medical malpractice.
