Stage 2 – Signs and Symptoms
Welcome back to my series addressing sepsis and why it is important to your cases. Feel free to email me with any questions you may have regarding the information I have provided so far or if you have questions regarding a case you are reviewing with one of these issues.
Today we are reviewing:
- What happens when SIRS involves Sepsis?
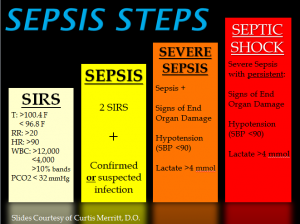
We know that Systemic inflammatory response syndrome (SIRS) is a serious condition in which there is inflammation throughout the whole body – an exaggerated defense response of the body to a noxious stressor, including infection.
- SIRS with a suspected source of infection is termed sepsis. Together they represent a physiologic continuum with progressively worsening balance between pro and anti-inflammatory responses of the body.
Sepsis is a life-threatening condition that occurs when the body’s response to infection causes organ injury. Sepsis is not a specific disease but rather a collection of symptoms resulting from an infection left unnoticed and untreated, and is a medical emergency requiring immediate treatment to reduce resident/patient morbidity and mortality. It is a race against time for nursing staff and medical providers as the residents/patients’ body begins to decompensate because of sepsis.
Because there are no specific tests to diagnose sepsis, it is imperative that nurses use critical thinking skills and know when to alert the chain of command or medical team to possible sepsis development.
Sepsis presents with worsening symptoms as the resident/patient continues to decline and decompensate. Paige Legal nurses know what symptoms to look for in developing symptoms of infection, which we then use to assess if standards were met in care. If overlooked or mistreated, sepsis can lead to septic shock, organ failure, and possibly death. Early recognition is crucial and key in halting sepsis progression to improve outcomes and decrease mortality rates. Paige Legal Nurse consulting has nurses ready to review the records to identify the events of your case and identify nursing actions taken (or missed).
What are the signs of sepsis?
- Fever:
- >100.4 F or <96.8 F may indicate a developing infection and should be monitored, with abnormal values reported to the medical team.
- However, in the elderly, a low temperature or hypothermia is a more frequent occurrence and maybe their response to infection.
- As we age our ability to generate a fever diminishes and becomes an unreliable sign of infection. Hypothermia (low temp <96.8 F) is an often overlooked or completely missed symptom of infection in nursing home residents.
- Mental/cognition changes:
- This includes any new or worsening confusion, lethargy, restlessness.
- Respiratory:
- Initial symptoms include tachypnea (>20 breaths per minute) or dyspnea (shortness of breath).
- Cardiovascular:
- Tachycardia (heart rate >100beats per minute) can also be a sign of sepsis.
- Genitourinary:
- Foley catheters with urine output less than 30 ml/hr. or 120 ml/4 hrs. (the threshold to meet for normal kidney function). In infection, this is a late-stage symptom.
- Decreased urine output – requiring assessment of incontinent resident/patient. How often are they urinating and what are the characteristics of the urine?
- This is a challenge to assess in dialysis patients because they already have decreased urine output.
- Skin:
- Does the resident/patient have pressure injury wounds, venous or arterial stasis ulcers, or surgical incisions?
- Does assessment of the skin reveal redness, cellulitis, or drainage?
- Lack of perfusion – is the skin cool and clammy, or discolored?
- Invasive devices:
- Assessment of intravenous IV catheters including skin surrounding the insertion site (should be free of redness).
- Foley catheters: when was it last changed? What does the urine look like? [clear vs cloudy, turbistop d]
- Labs if done:
- High or low white blood cell count?
Key facts:
- Nursing does not need a doctor’s order to do vital signs. These can be done at any time at nursing’s discretion as an assessment tool. Standard of care for nursing includes knowing when vital signs should be monitored and reporting results to the medical team.
- In a hospital, the medical team is readily available for the onset of abnormal vital signs (VS) to be directly reported. They are monitored every shift, on a routine basis.
- Abnormal VS are an early indicator and the standard of care would be for nursing [if an LPN] notify the supervisory RN and to promptly report any abnormal findings to the medical team.
- In a nursing home, also requires prompt notification to the RP with any acute change in condition.
Organ systems react to the presence of infection.
- Sepsis with one or more end-organs in failure is called Severe sepsis. Additional severe lab abnormalities are identified which include lactic acidosis, along with oliguria (lack of urine) and an acute alteration in mental status.
- When low blood pressure cannot be improved and continues as hypotensive despite intravascular (IV) volume repletion is called Septic shock.
In future posts will talk about the different areas most noted for sepsis development. I think you’ll find them educational and informative, and ultimately helpful in your cases involving sepsis and death.
Paige Legal Nurse Consulting is a Certified Legal Nurse Consulting firm with experienced acute care and nursing home nurses that are qualified to review cases involving infection and sepsis. Call 508-292-2372 or schedule your case development review online with us today!

Christie Paige MSN RN-BC LNC
Christie Paige is a Registered Nurse with over thirty years of experience. She brings her vast and extensive knowledge of clinical practice into the medical-legal arena as a Certified Legal Nurse Consultant. Mrs. Paige is the owner and senior nurse consultant of Paige Legal Nurse Consultants which specializes in Nursing Home cases focused on Sepsis, falls, pressure sore injuries and elder care medical malpractice.
