Stage 3 Severe Sepsis
Welcome back to my series of emails addressing sepsis and why it is important to your cases. Feel free to email me with any questions you may have regarding information I have provided so far or if you have questions regarding a case you are reviewing with one of these issues.
Today we are reviewing:
- Stage 3 – SEVERE SEPSIS
Previously we covered that nursing should be assessing every resident or patient for infection on a daily basis, shift by shift. We know that early detection of symptoms is the key for early treatment of any potential infection identified and that if left untreated can start a cascade of systemic issues. And that in Stage two: Sepsis is present when two of the mentioned SIRS signs are present, but there is also a confirmed or suspected infection present.
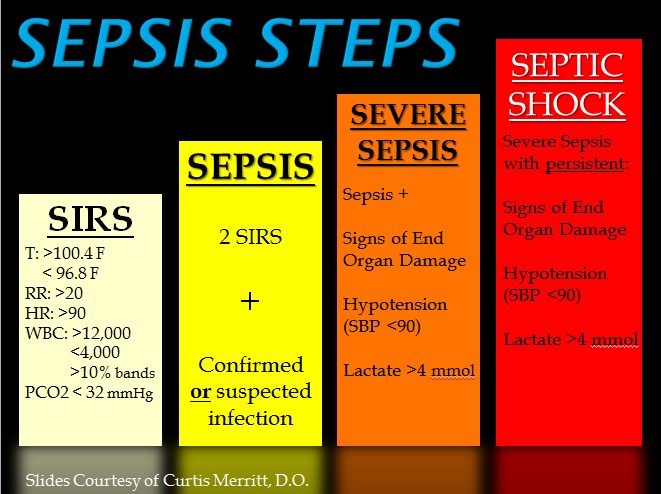
The third stage, called Severe Sepsis, is diagnosed when acute organ dysfunction begins. So now you have: Sepsis along with hypotension (low blood pressure) or hypoperfusion (decreased blood flow through an organ). Time is of the essence and early recognition is crucial and key in halting sepsis progression to improve outcomes and decrease mortality rates.
Remember the 2 most common issues that lead to sepsis?—- urinary tract infections and pressure injury wounds – Dehydration also plays into this– the elderly don’t drink enough– All of these are very common Nursing Home issues in case evaluation.
In many of our case reviews, we see Nursing just now recognizing symptoms, alerting the medical staff to symptoms and an order given to transfer the resident to the ER.
Our legal nurses are now evaluating the ER intake assessment for the abnormal findings, this includes their presentation on entering the ER, testing done with results and wrapping that information back to what was missed in the last days at the nursing home facility.
Sepsis treatment typically requires intravenous (IV) fluids and antibiotics. It is essential that the treatment begin as early as possible. The chance of sepsis progressing to severe sepsis and septic shock, causing death, rises by 4% to 9% for every hour treatment is delayed.
ORGANS IMPACTED INCLUDE:
- KIDNEYS – decreased urinary output- noted as dark concentrated colored urine; possibly foul smelling; progressing to oliguria (lack of urine); Serum creatinine starts to elevate; Acute Kidney Injury develops
- BRAIN – cognition impacted – a change in mental status; Glasgow score impacted
- HEART– increasing heart rate, lowering blood pressure, dizziness when standing
- LUNGS – increasing resp rate, oxygenation is negatively impacted
- LIVER- no outwardly signs but developing jaundice
- LABS note abnormalities: Elevated white blood cell count; lactic acidosis; liver enzymes;
- Also see decreased intake or appetite – leads to forced feeding at times >> Potential for aspiration
Key facts:
- Because there are no specific tests to diagnose sepsis, it is imperative that nurses do daily assessment for infection
- Nursing does not need a doctor’s order to do vital signs. These can be done at any time at nursing’s discretion as an assessment tool. Standard of care for nursing includes knowing when vital signs should be monitored and reporting results to the medical team.
- Only a doctor can provide a diagnosis of sepsis or septic shock.
- Organ systems react to the presence of infection.
- Sepsis with one or more end-organs in failure is called Severe sepsis.
- Dialysis may be required to remove toxins from the blood if the Kidneys are severely impacted. As the body heals, the kidneys may begin functioning again. But in many cases, organ damage is
- Up to 50% of sepsis survivors experience post-sepsis syndrome — long-term effects that can include severe muscle and joint pain, panic attacks, and decreased ability to sleep and concentrate which for attorneys– translates into PAIN & SUFFERING.
About one-third of sepsis survivors return to the hospital within three months of their discharge. The most common causes are repeat infection or sepsis.
