When Pressure Injury Wounds Results in Sepsis
Welcome back to my series addressing sepsis and why it is important to your cases. Feel free to email me with any questions you may have regarding the information I have provided or if you would like some help with one of your cases.
Today we are talking about Pressure injury wounds and the signs/ symptoms nursing should be looking for and assessing on a daily basis. You may be asking yourself what the standard of care for sepsis is for the LPN that works in a nursing home. We are going to cover that as well!
Did you know that skin is the largest organ in the body and serves as a barrier to pathogens and germs? A break on the skin surface becomes an opportunity for a localized infection that can quickly become systemic if not treated.
We know that elderly or bedridden residents/patients are at high risk for developing pressure injury wounds and therefore require attention to strategic preventative measures in their plans of care. This is nursing’s first line of defense in the prevention of pressure injury wounds.
Key facts:
- Any resident/patient at risk for skin breakdown should have a plan of care initiated with preventative interventions in place.
- Redness is a stage I pressure injury wound with standard nursing care requiring preventative interventions be initiated.
- A stage II pressure injury wound has broken the skin barrier and is now considered high risk for worsening.
- A key indicator of a worsening stage II pressure injury wound is the development of slough. Slough is not present in stage II pressure injury wounds only in stage III pressure injury wounds and higher (slough may be present in other types of wounds such as vascular wounds, diabetic wounds, and other non-pressure related wounds).
- A stage III, IV, or unstageable pressure injury wound requires emergent preventative interventions to be implemented as well as notification of the medical team (and RP in a nursing home). Nursing would expect to see a wound care consult followed by treatment of the wound by a team of wound care providers.
So how does the nurse assess a pressure injury wound for a developing infection?
Wound drainage is a key indicator. Nursing is expected to assess the amount of any wound drainage, any increase from previously identified drainage, the characteristics of the drainage such as consistency, color, odor, and the presence of pus, known as purulence (this can indicate infection). **If a staff nurse is not qualified to make these assessments, this strengthens the need for a wound care consult and treatment by a specialized wound care team.
Signs and symptoms of a pressure wound infection include:
- Erythema (redness or rash)
- Odor
- Pain
- Increasing wound drainage (may be yellow, green, brown, or blue)
- Fever, chills, nausea, vomiting (indicating the infection has become systemic)
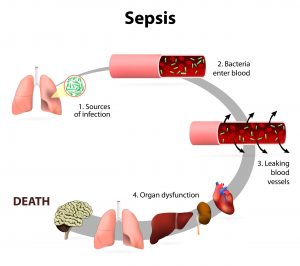
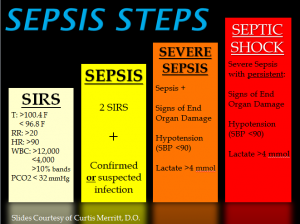
If a pressure injury wound becomes infected and is not appropriately treated, it will trigger SIRS and the cascade of sepsis. Click here to go to the blog reviewing SIRS and sepsis symptoms.
If sepsis remains untreated, it can evolve into septic shock.
Symptoms of SIRS and infection include:
- Fever >100.4 F or <96.8 F,
- Respiratory rate above 20 breaths per minute (tachypnea) or obvious shortness of breath (dyspnea),
- Heart rate above 100 beats per minute (tachycardia),
- Decreasing urinary output or decreasing episodes of incontinence,
- Change in mental status, typically noted as new or worsening confusion or lethargy.
Sepsis is a medical emergency requiring immediate treatment to reduce resident/patient morbidity and mortality. It is a race against time for nursing staff and medical providers as the residents/patients’ body begins to decompensate because of sepsis. Paige Legal Nurse consulting knows what assessment skills and clinical judgment nursing is expected to use for early detection and prompt treatment of developing of infection and sepsis. All nurses must use critical nurse thinking and prompt follow-up by using all available data such as physical assessments, vital signs, and tests performed to support the treatment of infection.
Resources
Paige Legal Nurse Consulting is a certified Legal Nurse Consulting firm with experienced acute care and nursing home nurses that are qualified to review cases involving infection and sepsis. Call 508-292-2372 or schedule your case development review online with us today!

Christie Paige MSN RN-BC LNC
Christie Paige is a Registered Nurse with over thirty years of experience. She brings her vast and extensive knowledge of clinical practice into the medical-legal arena as a Certified Legal Nurse Consultant. Mrs. Paige is the owner and senior nurse consultant of Paige Legal Nurse Consultants which specializes in Nursing Home cases focused on Sepsis, falls, pressure sore injuries and elder care medical malpractice.
